Despite a shortage of 109,000 nurses predicted to hit Australia by 2025, thousands of new graduate nurses and midwifes struggle to find employment each year. The resulting bottleneck is locking out the next generation and taking away their right to supportive transition into the workforce. As many graduates ponder their future, Robert Fedele investigates the complex and critical dilemma facing the profession.
Jessica Westmoreland is all trained up with nowhere to go. After finishing high school she pursued a career in nursing, undertaking a three-year degree at the University of South Australia and eventually graduating in March, 2015.
Subscribe for FREE to the HealthTimes magazine
Regrettable, the 21-year-old currently belongs to a disillusioned cohort of nursing graduates unable to find work. “It’s been a year and a half that I’ve been applying for jobs full on. I will keep applying for nursing jobs but I am considering going into another field.
As much as it’s what I wanted to do, if I knew from the start that this is what was going to happen I wouldn’t have even bothered. “
Like many students, Jessica thought landing a job as a nurse would be straightforward given the outlook of a looming workforce shortage on the horizon.
But these days her mood has swung to disbelief as she continues to struggle to find a permanent job.
As the end of her degree approached in late 2014 Jessica began methodically applying for graduate placements. She applied for a position within SA Health, hoping to snare a spot at one of the state’s public hospitals, but was unsuccessful. She applied anywhere and everywhere, including interstate and in rural and remote areas. Again she came up short.
An interview with a public hospital in Sydney appeared promising but ended in another knock back due to ‘excessive applicants’.
Last year alone, Jessica estimates she applied for more than 300 nursing jobs. “I just want something. I want to be in a theatre eventually but I understand I’m not going to get that straight away.
Whether I work up from aged care, I don’t care. I just want to start off as a nurse.”
In November last year, Jessica was offered a three-year graduate position at an aged care facility in Melbourne. Packing her bags she left home for the first time to follow her dream. But the move quickly turned sour and she soon returned to Adelaide.
“It was a full-time contract but once I got over there they only gave me 16 hours and they said for the first two years I’d be a carer and the last year and RN. I was like ‘Well hang on, that’s not what you told me when I came over here”, she says. “I couldn’t afford to pay my rent or eat pretty much so I stayed there until I could and just got back home at the start of the year (2015). I’ve been working as a cleaner, kitchenhand and waitress ever since.”
Walking Away
Jessica’s story is not uncommon and supports a rising problem.
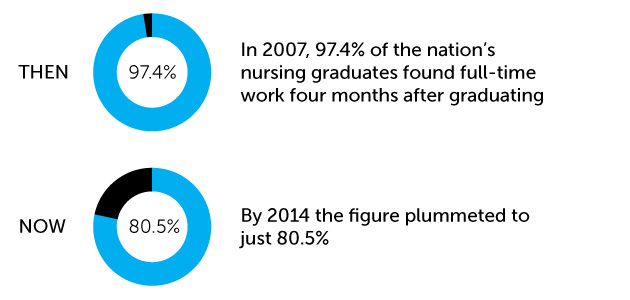
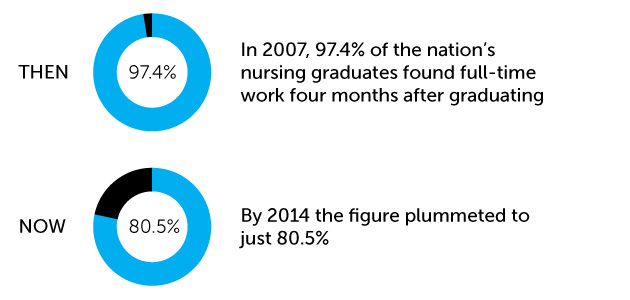
Latest figures released by Graduate Careers Australia (GCA), which conducts an annual survey examining the fate of graduates four months after the completion of their qualifications, reveal a steady decline over the past decade in the number of nursing graduates who manage to find full-time jobs.
In 2007, 97.4% of the nation’s nursing graduates found full-time work four months after graduating. But by 2014 the figure plummeted to just 80.5%.
Queensland resident Chantelle, who studied nursing at Griffith University and graduated in December last year, claims just half of the 300 students in her intake found jobs. Chantelle was one of the unlucky ones.
“I’m freaking out. I live on my own and I don’t have a job now,” she says. “I’ve done heaps of placements that I didn’t like. Staff treated me horribly but I pushed through and finished the degree and now I have nothing to show for it.”
Chantelle is keen on securing a role within mental health nursing but has been unsuccessful so far.
Last year she begrudgingly turned to agency work, assuming the role of an assistant in nursing at an aged care facility. But she quickly became overwhelmed by the lack of support and quit. “I just didn’t want to do something that I’ll end up hating and will make me not want to do nursing at all.
“You’re put on a different area every shift. You don’t know where you’re going to go or who you’re going to meet. Being a grad I have no idea what I’m doing.”
Chantelle’s struggles have forced her to reconsider her place in the profession. She now regrets pursuing nursing and says she has “nothing to look forward to”.
International student Ranjit Dhillon is another graduate at the crossroads.
The 31-year-old mature age student from India studied nursing and Flinders University in South Australia, graduating in December last year.
Ranjit completed placements in general medicine, theatre (OT) and orthopaedics throughout her degree, but says potential employers still grill her credentials.
Ranjit, who has applied for permanent residency, spent almost $60,000 to complete her degree.
She is currently working as a carer across nursing homes in South Australia and will keep plugging away for a little while longer. “I think I’ll keep going for another six months. But I’m not interested in any other field or other jobs. I just want to be a nurse.”
 Pinpointing Problems
Pinpointing Problems
In late 2014, the Australian Nursing and Midwifery Federation (ANMF) pulled together dozens of nursing and midwifery leaders and key stakeholders for a Roundtable to canvass strategies to help around 3,000 graduates who miss out on jobs each year.
Progress lead to the ANMF surveying new graduate nurses and midwives late last year in a bid to gain clearer insight into their employment experience.
The information yielded will provide a platform for debate at a second Roundtable to be held this year in Melbourne.
Shedding light on the ‘growing’ problem, ANMF Assistant Federal Secretary Annie Butler blames the workforce bottleneck on a cluster of triggers ranging from budget cuts, the global financial crisis, the impact of migrant labour, poor workforce planning and an overarching disconnect between governments, universities and hospitals.
The obvious complexity of the issue has helped fuel conflict among key stakeholders regarding the extent of the problem and exactly who is responsible, she adds.
“We believe that it’s not just one single thing that is at fault,” Ms Butler says categorically. “There’s a number of factors. Governments come and go. Governments don’t care about the long-term. Governments care about short-term, politically expedient solutions, by and large.”
Ms Butler elaborates, pinpointing an inability to spark dialogue with governments as well as private employers, many of whom run very successful graduate programs, as an ongoing barrier to achieving progress. “We’re trying to get employers to tell us how many graduates their taking in 2016, whether they could take more, what is stopping them and what would help them.”
Ms Butler admits the employment of foreign workers under the temporary 457 visa scheme is having an impact on available positions in some areas.
“We don’t have a genuine skills shortage. What we have is some employers saying to us that they’re using 457 visa workers because they don’t have the resources to support the new graduates.”
She is hopeful the ANMF’s upcoming Roundtable will renew focus and prompt the development of a national framework to tackle the problem.
Importantly, Ms Butler says one the biggest objectives will entail attempting to collate and examine an extensive range of diverse data sets for the first time.
“Findings ways of getting as many of the graduates into the workforce right now and keeping them there is critical,” she says.
“If we’re not getting these people into employment and educating them we’re going to have this massive shortfall in our skilled workforce.”
The impact of 457 visa workers
A Parliament Inquiry, launched in June last year, is currently examining the impact of skilled migrant work programs on Australia’s workforce.
The ANMF provided an extensive submission to the Inquiry and appeared before a public hearing in Melbourne where ti called for changes to the 457 scheme that would safeguard the employment of local graduates.
The 457 visa program was devised to engage temporary migrant workers to fill unexpected shortages but the ANMF insists the scheme is being misused by some employers and making it tougher for nursing and midwifery graduates to find a job.
“We believe that it’s being taken as a shortcut and that employers see it as a quick fix,” ANMF secretary Annie Butler said.
ANMF Senior Federal Industrial Officer Nick Blake, who also appeared before last year’s hearing, urged the committee to consider several recommendations to fix the widespread problem.
Chiefly, Mr Blake suggested a one-for-one rule, where employers would be required to hire a graduate for every 457 worker they employ. “While the ANMF continues to support migration, our union, along with most nursing and midwifery professionals and regulatory authorities, are increasingly concerned of the negative impact the high numbers of temporary migrant workers are having on the employment opportunities of domestic graduate nurses and midwives.”
The committee tabled an interim report to the Senate last October and the Inquiry has now been extended.
A public hearing will next take place in Canberra in early February as the issue is further explored.
Budget Blues
When government dollars get stretched it is invariably the health system which gets hacked first.
The outcome results in fewer beds equalling fewer places for nurses.
In Tasmania, the landscape has remained in a precarious position since budget cuts in 2011 drastically reduced beds. Today, almost half of the state’s 300 annual graduates struggle to secure a graduate position.
Queensland experienced similar hurdles until a change of government last year spurred a revival. The state government has guaranteed funding for 1000 new graduate positions every year over the next four years under a $111 million plan.
The funding intertwines with the government’s promise to legislate nurse-to-patient ratios, set to be carried out in stages from July.
The upturn appears promising across the board, with the Sunshine Coast Hospital and Health Service (SCHHS) employing a record number of nursing graduates for 2016 under its Graduate Registered Nurse program. More than 80 new graduates will begin their 12-month program this month and be placed on rotation throughout medical and surgical wards at hospitals including Caloundra and Gympie.
As Queensland climbs from the depths, ANMF (Tas Branch) Acting Secretary Caroline Saint proposes her state look at alternatives such as implementing shorter graduate placements for larger numbers can be rolled over. “Many new nurses believe the graduate year is important and should be undertaken – preferably in the acute sector. The private sector as well as the aged care sector have some limited placements for graduate programs. It might be better to have a shorter transition program which would allow a larger number of graduates to get experience, rather than running for a full-year for the half of the students.”
Ms Saint says workforce issues currently plaguing the state are having an untold impact. “Don’t fear the loss of a generation of nurses. But we could lose many very capable nurses who, if they cannot get early experience, may start to lose confidence in their ability to work in the health system.”
Global financial crisis
Asked to consider reasons behind the graduate conundrum, Queensland Nurses’ Union (QNU ANMF QLD Branch) Secretary Beth Mohle identified the global financial crisis as the leading cause behind her state’s challenges.
“The turnover, in Queensland Health particularly, really fell off a cliff,” she recalls. “It dropped significantly so there was understandably less places for graduates.
“There was always going to be this hump of new graduates coming through who we would need in a few years’ time but because of the global financial crisis in 2008, a lot of our older nurses put off their retirement because they took a big hit.”
As the state’s situation improves, Ms Mohle admits many graduates who failed to find jobs in the murky years of 2012 and 2013 have most likely been irreversibly disconnected. “No one keeps good data so they’re lost to the system. Some went to the private sector, but not many. Some went interstate. Some went overseas. Some went to NSW to meet their increased numbers for ratios. Some actually left nursing and midwifery altogether and undertook further education in another field. This is the incalculable human and systems cost of not having a proper plan.”
Ms Mohle welcomed the Queensland government’s recent funding investment in new graduates, but stressed the need to back it up with ongoing support and mentorship if long-term change is to occur.
Finding Solutions
According to ANMF Assistant Federal Secretary Anne Butler, creative thinking, the development of innovative models, and national collaboration, underline the primary ways to solving the problem.
The ANMF continues to spruik potential strategies like waiving HECS fees for graduates who accept employment in areas of high need, such as rural and remote health; and establishing solid partnerships between large metropolitan hospitals and rural hospitals, and similar relationships between hospitals and primary health networks.
Ms Butler says evidence of encouraging change is emerging, with some hospitals, for example, implementing specific casual pools for graduates unable to secure a formal placement in a bid to keep them connected in the profession.
St Vincent’s Hospital in Melbourne is one such hospital making inroads.
The hospital appoints about 115 graduates each year, receiving funding from the Victorian government for the first 10 graduates and a percentage from there on.
“We interviewed 500 and we took 115,” says Deanne Riddington, Director of the hospital’s Nursing Education Centre.
“We interview a lot because we want to meet them. It’s very labour intensive but we want to meet them. We don’t want them to be a name on a piece of paper.”
Ms Riddington sits on the hospital’s nurse executive, which regularly dissects nursing numbers and workforce patterns on a broader level.
One of St Vincent’s newest strategies involves its Care of the Older Person Graduate Nursing Program, a specialised aged care pathway that offers an alternative option to graduates who miss out on the hospital’s mainstream acute program.
“We’ve noticed a niche and we’ve got graduates coming in that way,” Ms Riddington explains. “It gets them into St Vincent’s. It gives them career opportunities down the track. Whether they stay in aged care is completely up to them. We want people to stay full stop. Like a typical big hospital, there’s lots of opportunities when they finish their graduate year to play in the diversity of healthcare.”
Ms Riddington’s core advice to future graduates centres around getting exposure to as much robust, diverse and engaging clinical placement as possible. “I think there’s a responsibility that the universities have to ensure the student has lots of opportunity to consolidate because it’s the clinical skills and communicating with patients that matters. They’ll be able to do anything if they can that well.”
Opening Doors
Professor Maxine Duke, Head of the School of Nursing and Midwifery at Deakin University, agrees that clinical placements can pave the way to future employment.
The university maintains formal partnerships with seven healthcare organisations across Victoria.
“We try and work with our clinical partners and have the students keep going to those placements for a great deal of their course so that they’re familiar with the organisation and the organisation is familiar with them,” Professor Duke says. “So when it comes to choosing students they’re likely to choose ones they have experience of.”
Deakin University operates across three campuses and takes in about 700 nursing students each year.
According to figures, about 87% of the university’s nursing graduates find jobs after completing their degree, ranking the school among the nation’s leaders.
Professor Duke says students are thoroughly drilled on making the transition from university to the workforce and encouraged to consider a range of entry options.
“We talk about opportunities other than the metropolitan area and acute tertiary hospitals. We talk about rural and interstate. Some of our students find employment very easily in Perth and so forth,” Professor Duke explains.
“The majority [of students] still feel they should be in an acute setting to consolidate but that’s a historical, cultural artefact. Sub-acute is now as acute used to be and acute is intensive care these days.
“And aged care has incredible opportunities for nurses. Within a very short time they’ll move through the ranks to doing case management or leading teams much quicker than they would in an acute environment.”
Professor Duke believes the shortage of places for graduates has improved since the easing of the global financial crisis.
She said it is now incumbent on all key stakeholders to work together to promote careers across the health service in places such as mental health and aged care in order to debunk traditional perceptions regarding the need to complete a graduate year in an acute setting.
Don’t give up
Despite the graduate situation persisting, ANMF Assistant Federal Secretary Anne Butler remains optimistic.
“Stick it out. Come to us. Tell us your story. Let us know what your circumstance is so that we can find out more ways to try and help,” she says.
In the same vein, while the short-sightedness of governments and lack of funding may rightly be to blame for the crisis, there’s one fundamental area perhaps still often overlooked in the battle to find a job: diligence and luck.
Registered nurse Tori Burek is testament to the adage persistence pays. Tori experienced the feeling of isolation and soul-searching first-hand after completing a nursing degree at Victoria University’s St Albans campus in October, 2014. Her failure to secure a graduate position left her flattened and wondering where she had gone wrong. Over the next six months Tori applied for hundreds of nursing jobs but kept getting rejected.
“It was six months’ long of constantly going to work, coming home, and applying for jobs. It gets a bit tedious after a while and you come to a point where you think ‘is it even worth it?”
During the state of limbo, Tori kept connected by undertaking training courses offered by ANMF, agency jobs, and non-nursing jobs.
In a stroke of good luck, Tori was able to secure a graduate position at St Vincent’s Hospital in Melbourne via a mid-year intake. She finally began her career as a nurse last September, starting off on the orthopaedics ward.
“It sounds clichéd but I really do think everything happens for a reason because in that six months I learned to work harder and to pick myself up, and everything I learned about nursing in that time will help me now as well. So I don’t regret that time.”
Reflecting on her journey, Tori’s message to graduates confronting similar uncertainty is simple: keep persevering.
She says she feels humbled to work at St Vincent’s and is looking forward to a long career. “The thing I love most is the place I’m working at. If you come to work every day with people who are as passionate as you are then it makes the whole difference.”
Reprinted with permission of the Australian Nursing & Midwifery Federation